Applying guidelines in actual clinical nursing practice in New Zealand
11 May 2015
Kia Ora from your urological New Zealand nursing colleagues. We hope you had a highly successful congress in Madrid. It has been four years since I joined in Vienna, yet my memories of a very worthwhile, stimulating meeting are still vivid. I hope to join another EAUN annual meeting but it can be challenging to get release time and funding to attend even local meetings, let alone meetings held on the other side of the world!
My EAUN membership remains important to me, as does my membership to our national organisation the New Zealand Urological Nurses Society. Both organisations regularly publish a newsletter to provide a vehicle for networking with colleagues, as well as new information on urological topics, case studies and literature reviews.
You can be very proud of the comprehensive EAU and EAUN guidelines which are excellent evidencebased resources available for consultation when planning care for urological patients and when preparing teaching sessions. I recently delivered a case review to a group of non-urological nursing colleagues, evaluating the care delivered to an elderly lady with recurrent urinary tract infections. When critiquing the care delivered I used the recently updated EAU Urological Infections guideline as a reference.
While New Zealand local microbial environment and resistance patterns vary somewhat from those of the Northern Hemisphere, the evidence-based principles for treatment of urological infections certainly apply. As outlined in the Urological Infections Guideline, prescribing decisions should be guided by a prudent use of available antibiotics, based on local pathogen and susceptibility profiles. These principles apply not only for treatment of urological infections but also in the area of prophylaxes.
“The document stresses the need to carefully assess risk factors for sepsis including an individual’s risk of carrying resistant bacterial strains”
EAU Urological Infections guidelines note the high risk of infection associated with transrectal prostate biopsy and strongly recommend antimicrobial prophylaxis. The document stresses the need to carefully assess risk factors for sepsis including an individual’s risk of carrying resistant bacterial strains (i.e. fluoroquinolone (FQ) resistance). As detection of FQ resistant E.coli and ESBL E.coli or Klebsiella sp in our setting is relatively common, the Waitemata District Health Boards Urology and Infectious Diseases Departments implemented regional guidelines whereby all men undergoing transrectal prostate biopsy have rectal swabs taken prior to the procedure. A targeted single dose of prophylactic antibiotic is then prescribed in response to the rectal swab culture result. At present the oral antibiotic regimes in use are Ciprofloxacin monotherapy, Ciprofloxacin with Cotrimoxazole or Fosfomycin.
At Waitemata District Health Board, the urology clinic nurses prospectively collect data on every patient who undergoes a transrectal ultrasound-guided prostate biopsy, including recent travel history and antibiotic use. When men present for their prostate biopsy results (10-14 days post-procedure) data is again collected, this time recording any uncomplicated urinary tract infections or urosepsis events (positive blood cultures) that occurred post-biopsy.
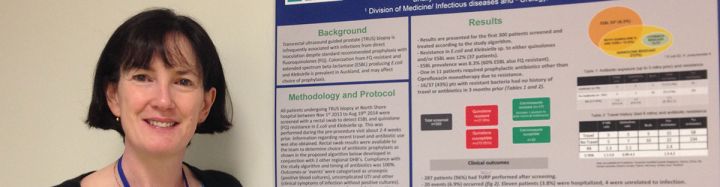
Data is also captured on men who experienced clinical symptoms of infection without positive cultures. Results from the first 300 patients were recently presented in a poster presentation at the Australasian Society of Infectious Diseases Annual Scientific Meeting (March 18 to 22) held in Auckland. Data analysis revealed our population’s ESBL prevalence rate to be 8.3% (60% ESBL also FQ resistant). One in 11 men required prophylactic antibiotics other than ciprofloxacin monotherapy. Through the use of targeted antibiotics no ESBL infections occurred post-transrectal prostate biopsy.
Such audits enable our team to contribute to the national and international evidence-based that will inform future prophylaxis guidelines. The data collection process requires diligence, enthusiasm and the collective will of many. Analysis of the data requires similar characteristics, as well as thorough and close scrutiny to ensure the data is ‘brought to life’ and contributes to patient care decisions moving forward.
Excellence in patient care drives the content of our organisations newsletters. It is the main goal of the EAU/EAUN guidelines and has been the focus of most, if not all, of the 2015 EAUN congress sessions.
I sincerely hope those of you who were at the meeting have benefited from the lectures. And who knows maybe I can join next year!
Sue Osborne
Urology Nurse Practitioner
Waitemata Disrict Health Board, Dept. of Urology, Auckland (NZ)
Sue.osborne@waitematadhb.govt.nz
European Urology Today Vol. 27 No. 2 March/May 2015

