Insights on best practices: EAUN fellowship at Dutch cancer centre

For the last five years I have been working as a charge and urology ward nurse at Mater Dei Hospital in Malta which is the country’s only acute general university teaching hospital that offers full-range hospital services.
Since my nursing registration in 1982, I have always worked in the acute general hospital of Malta although for 28 years I worked mainly in the obstetrics, gynaecology and Neonatal Intensive Care departments. Thereafter, I worked at the Adult Urology Department.
Mater Dei hospital provides an extensive range of specialist services including urology. The Department of Urology has four consultants, two wards with 36 beds, a nurse-led outreach service and a preoperative assessment unit. Our urologists use the general outpatients department and operating theatre for outpatient’s visits and surgical interventions. We do not have a urology department that caters specifically for procedures related to urology since other minor interventions such as flexible cystoscopies, prostate biopsies and ESWL are done at the day care theatre. Urology Ward 2, where I am assigned, is an 11-bed inpatients mixed ward and I am supported by 11 senior professional nurses who have a vast experience in urology and a support staff. We have a 1:6 patient-nurse ratio allocation.

Fellow Helen Attard Bason from Malta (left) with mentor Corinne Tillier from Amsterdam (right)
For the last five years, since I started working in the urology department, I had been running the Intravesical therapy and the bisphosphonate treatment for prostate cancer patients with bone metastasis. My aim is to further develop this service especially with regards to the training of the staff who administers such a therapy. Although my staff are very competent and have the necessary expertise to administer treatment, they are still not recognised as competent practitioners to administer intravesical treatment as required by international guidelines.
EAUN Fellowship
My applying for EAUN fellowship was motivated when I realised that delivering the highest standard of urological nursing can be best achieved through the exchange of best practices and the application of guidelines in hospital practice, one of the main goals of the EAUN. Moreover, I believe that having the opportunity to observe a nursing team in another European country is a great learning experience which can help improve one’s own practice and nursing skills.
Finding out what differentiates the uro-oncology practice at Antoni van Leeuwenhoek (AVL) Hospital from our practice at Mater Dei Hospital was high on my agenda since this will inform my work with urology cancer patients. Furthermore, I also believe that as the complexity of the healthcare delivery system increases, the need to intensify the knowledge through research, networking and exchange of best practices is crucial. I had applied for the Netherlands because AVL Hospital specialises in uro-oncology and I would like to apply the best standards of care in our department. Besides I also believe that crossing the borders across the EU to experience another environment in healthcare systems would eventually benefit my organisation and help me build contacts for learning and practice exchanges.
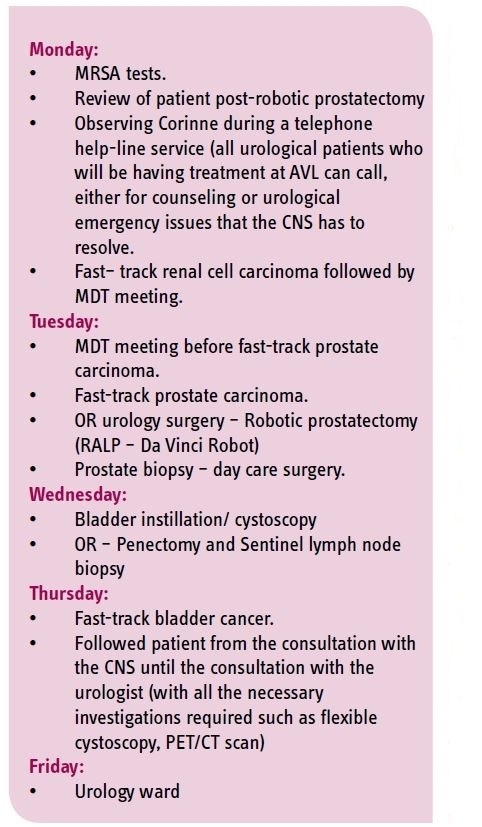
First, I would like to mention the remarkable organisation of my visit at AVL hospital, which was well-prepared by Ms. Corinne Tillier, a Uro-Oncology Clinical Nurse Specialist (CNS) responsible for localised prostate and renal cancer patients, and who also chairs the EAUN’s Scientific Congress Office. I had also worked with CNS Jolanda Bloos-van der Hulst who is responsible for bladder and penile cancer patients and current chair of the network urooncology nurses in North Holland. Working with Corinne and Jolanda were Eva Offringa, a CNS student (another year and she will have the title of MANP) Master Advanced Nursing Practice – good Luck Eva!) and CNS Erik Van Muilekom, past president of the EONS. My fellowship programme schedule from
September 26 to 30 consisted of the following:
The host institution
The Netherlands Cancer Institute and the Antoni van Leeuwenhoek (AVL) Oncology Hospital is the only dedicated cancer centre in The Netherlands and maintains an important role as a national and international centre of scientific and clinical expertise, development and training. The Antoni van
Leeuwenhoek Hospital has 185 medical specialists, 45 Clinical Nurse Specialists, 180 beds, an outpatients clinic with around 106,000 visits, 12 operating theatres and 11 irradiation units for radiotherapy. This oncology centre offers a state-of-the art oncology specialists’ consultation that is made up of a multi-disciplinary team (consisting of an oncology and urology clinical nurse specialists (CNS), a clinical urologist, a clinical oncologist, radiologists, radiation oncologists and a pathologist). Such services are integrated with compassionate care for clients visiting the AVL hospital. The urology ward is integrated within the surgical department and deals with conditions related to both female and male pelvic organs (urology and gynaecology).
It is impressive how nursing care in this hospital is provided in a friendly, caring and a quiet environment, and there is an emphasis on effective communication especially with the patients and their families. Although there was a time when I could not understand what was being said with the patient because of the language barrier, I, however, noted the sense of satisfaction and collaboration within the nurse-patient relationship. All the staff made me feel welcome and they also tried to explain (in English) what was being said so that I can understand and follow the conversation.
Effective communication was also evident between the physician and the uro-oncology nurse specialist at AVL. A close working relationship exists between nurses and physicians. There is a physician-nurse team collaboration environment with an open attitude, mutual respect and trust which facilitates the decisions taken by the CNS. This mutual collaboration was also evident during the multidisciplinary meetings that were held regularly to plan care and treatment. As an outside observer and with the language barrier, it was difficult for me to identify who was who during the meeting because all the members had collaborated well together. However, the CNS whom I was observing gave a quick account of the patient’s history. She also has the task of informing her clients about the decisions taken on their care pathway. The CNS has an important role in the care pathway starting from the first referral and down to the follow-up and any post-surgical intervention. I had followed the CNS during a telephone advice line and during a CNS-led preadmission clinic where newly referred patients can discuss their concerns and when their care pathway would be explained before any other investigations and surgical interventions are performed.
Learning points
From this experience not only have I reached my objectives but have also reflected on the importance of networking in nursing. This fellowship has also helped me in analysing the level of care that we deliver in our country compared with other European countries. Furthermore, sharing information whether it is clinical, administrative or research-based is necessary and can benefit or help improve our healthcare system. I have also realised that through networking, we can break our comfort zones and become key players in healthcare.
One important observation that I had was the fast-track cancer diagnosis which in Malta is only applicable for colorectal cancer. If introduced locally within the urology specialty, this system can be beneficial because not only will it minimise the waiting time for the patient to receive treatment but it will also reduce patient anxiety which follows after a cancer diagnosis.
Throughout the fast-track service after patients are referred by other hospitals or their GP, and within the first 24 hours of referral, the CNS will organise everything for the patient including the appointment for assessment, the required scans/ MRI and biopsies after which the results are discussed in an MDT meeting. These are very often done within the same day and during the MDT a treatment plan is prepared and proposed to the patient. It means that patients in one day would know the definitive diagnosis and stage of her/his disease and which treatment the MDT has advised. This minimises the trauma and anxiety for patients and their families. Every year about 210 patients with bladder cancer, 60 with penile carcinoma, 680 with prostate cancer and 160 with renal cell carcinoma are seen at AVL hospital’s fast-track urology cancer pathway.
Finally, I would like to thank everyone, especially all the team members involved in organising my visit at AVL hospital, for their warm welcome, and particularly Corinne Tillier who really went out of her way to mentor me and make my visit truly productive. The experience I gained will surely boost my knowledge with regards uro-oncology and the way I organise patient care. I would really encourage everyone to apply for a fellowship programme. Last and not the least, my sincere gratitude to the EAUN for this great opportunity.
Helen Attard Bason, Rn , Urology Department, Mater Dei Hospital, B’kara (MT), helen.attard-bason@gov.mt

