Personalised risk prediction of side effects after RARP
Helping patients to make better treatment choices
Specialising in prostate cancer, I have worked as a nurse practitioner in urology for the last 13 years. I have seen many patients with localised prostate cancer have difficulties to make a choice of treatment.
Many treatment options are available and are dependant of prostate cancer staging categories, grading classification and PSA level [1] (Table 1). Regardless of the treatment options chosen, most patients (>95%) with localised PCa are still alive at 15 years and only 2.7% will die from PCa.[2]
In my practice I often hear patients complaining about the standardised information we give to them to help make a treatment choice. Most of the information about the side effects of treatments are indeed standardised and largely based on previous clinical studies and patient cohorts from high volume specialised PCa centres. [5] Many patients doubt their preferred treatment choice and some of them (3-4%) even do regret their choice. [4]
When Dr. N. Grivas (GR) joined our hospital for a PhD, we began to collaborate, and he inspired me about individualised predictive factors of side effects after RARP. I spoke to Prof. Van Der Poel (NL) who encouraged me to begin a PhD about this subject.
I was able to combine a PhD with my clinical work and dedicated one day a week to my research. Now after three years, I am analysing the results of my last clinical research and I hope to finish my PhD at the end of 2023. In the meantime, I have already presented some results of my research at the EAU Congress (European School of Oncology Session) and also at the International Society for Quality of Life Research (ISOQOL) congress.
Helping patients in their choice is always a priority for me (shared decision-making). I use the Patient Reported Outcome Measures (PROMs) as a basis for interviews with patients. The results of the PROMs are important to evaluate quality of life (QoL), lower urinary tract symptoms (LUTS), and status urinary continence, erectile function, as well before treatment (baseline) as in follow up after treatment of PCa.
My thesis is divided into several sections:
1. PROMs in clinical practice
PROMs play an increasingly important role in the planning and evaluation of medical care. A high response rate is crucial to get a good view of the patient population. QoL questionnaires in oncology are important in order to evaluate the impact of the disease or the treatment of cancer patients and guide treatment decisions. The traditional way to collect data is a paper-based questionnaire sent by post. However, online questionnaires seem an attractive and cheap way to send a survey. The response rate of PROMs is higher when a reminder paper-based questionnaire is sent to the patients who do not respond to the web-based questionnaire. Elderly patients respond significantly more often than younger patients to both questionnaires (web-based or paper-based). [6]
PROMs are widely used after robot-assisted radical prostatectomy (RARP) in order to evaluate the impact/burden of the treatment. The most bothersome side effects of RARP are urinary incontinence (UI) and erectile dysfunction (ED). During the follow-up consultations, clinicians (urologists and nurse practitioners) report these side effects in interviewing patients. Discrepancies between PROMs and clinical report outcomes (CROs) are known [7] but it is not clear if it has an impact on management of UI and ED after RARP.
Results indicated that clinicians overestimated ED and underestimated UI compared to PROMs, but the observed discrepancies between the PROs and CROs did not affect offered management and counselling of UI and ED. [8]
2. Preoperative predictors
The extent of nerve preservation or fascia preservation (FP), the preoperative membranous urethral length (MUL) and the inner levator muscle distance (ILD) have been reported to affect continence recovery following robot-assisted radical prostatectomy (RARP). [9] Individualised information about the risk of UI after prostatectomy could help patients in shared decision-making.
The continence prediction tool (CPRED) was developed based on MUL, ILD and FP Score 0 (no erectile nerve sparing). We compared a historical cohort that received standardised information about risk of UI after RARP and a prospective cohort that received individualised information about risk of UI voiding complaints was associated with grade 2–3 leakage on cystography in cohort but not in cohort A. Grade 2–3 leakage on cystogram was more likely in men with larger prostates and preoperative voiding complaints. Selective cystogram in men with larger prostates and preoperative lower urinary tract symptoms (LUTS) may prevent early AUR and voiding complaints after RARP when prolonged TUC use is applied. [12] In the practice we now perform a cystogram after RARP only in patients with high risk of anastomosis leakage after RARP.
3. Comprehension of predictive factors by patients
In my thesis we focused on pre-, per-, and post operative predictive factors in order to help patients with PCa. However, it is primordial to know how to communicate the predictive factors to patients. As healthcare professionals (HPs), we tend to speak in percentage with patients. How could we be sure that patients do understand the real risk of urinary incontinence after RARP? Patient consultations with nurse practitioners and urologists discussing personalised risks of UI after prostatectomy were audiotaped, transcribed, and coded. HPs always used percentages, but rarely used natural frequencies (14%). Uncertainty was disclosed in only 34% of consultations. One-third of patients used personalised risks in their treatment decision making by either switching to another treatment or sticking to their initial preference. Patients value and use personalised side-effect risks during treatment decision-making. Clearly explaining the relationship between risk factors and personalised risk (CPRED score). Patients who received the individualised information switched more often from treatment options than patients in historical cohort. Personalised information about the risk of UI after RARP makes more patients reconsidering their initial treatment preference. The CPRED correlated strongly with continence outcome after RARP and is a useful tool for shared decision-making. [10]
The recovery of ED after RARP is also very important for patients. My last clinical research is on non-surgical predictive factors of ED after RARP. It will be innovative if we can show that some non-surgical factors have an impact on the recovery of ED after RARP and if patients could have a direct influence on factors to recover from ED after RARP.
4. Postoperative predictors
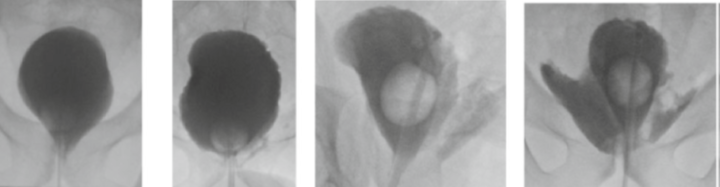
The role of a cystogram to assess the vesicourethral anastomosis (VUA) after robot-assisted laparoscopic radical prostatectomy (RARP) has been debated. Early catheter removal without cystogram was reported to be associated with a trend towards an increased risk of acute urinary retention (AUR). Leakage was scored according to Williams and Menon [11] (See Fig. 1).
A cohort of 1390 men (cohort A) that routinely underwent a cystogram after RARP was compared to a group of 120 men (cohort B) that underwent cystography 7–10 days after RARP but had the transurethral catheter (TUC) removed independent of cystography findings. The incidence of AUR and estimates may help patients understand and recall those. HPs should not only give patients specific and precise numerical risk information, but should also put effort in explaining how the personalised side-effect risks are determined. [13]
Conclusion
My PhD is focused on the pre-, per-, and post operative predictive factors of side effects after RARP and I hope that the results of my research will help patients to make a better treatment choice without regrets.
Mrs. Corinne Tillier, MSc, PhD stud. Netherlands Cancer Institute, Antoni Van Leeuwenhoek Hospital, Amsterdam (NL)
References
1. https://uroweb.org/guidelines/prostate-cancer
2. Hamdy FC, Donovan JL, Lane JA, Metcalfe C, Davis M, Turner EL, Martin RM, Young GJ, Walsh EI, Bryant RJ, Bollina P, Doble A, Doherty A, Gillatt D, Gnanapragasam V, Hughes O, Kockelbergh R, Kynaston H, Paul A, Paez E, Powell P, Rosario DJ, Rowe E, Mason M, Catto JWF, Peters TJ, Oxley J, Williams NJ, Staffurth J, Neal DE; ProtecT Study Group. Fifteen-Year Outcomes after Monitoring, Surgery, or Radiotherapy for Prostate Cancer. N Engl J Med. 2023 Apr 27;388(17):1547-1558. doi: 10.1056/NEJMoa2214122. Epub 2023 Mar 11. PMID:36912538.
3. van Stam MA, Aaronson NK, Bosch JLHR, Kieffer JM, van der Voort van Zyp JRN, Tillier CN, Horenblas S, van der Poel HG. Patient-reported Outcomes Following Treatment of Localised Prostate Cancer and Their Association with Regret About Treatment Choices. Eur Urol Oncol. 2020 Feb;3(1):21-31. doi: 10.1016/j. euo.2018.12.004. Epub 2018 Dec 26. PMID: 31411965.
4. Violette PD, Agoritsas T, Alexander P, Riikonen J, Santti H, Agarwal A, et al. Decision aids for localized prostate cancer treatment choice: Systematic review and meta-analysis. CA: a cancer journal for clinicians. 2015;65(3):239-51
5. Howell D et al (2015) Patient-reported outcomes in routine cancer clinical practice: a scoping review of use, impact on health outcomes, and implementation factors. Ann Oncol 26(9):18461858
6. Tillier CN, van Stam MA, de Blok W, van Muilekom HVM, Bloos-van der Hulst J, van der Poel HG. Web-Based Quality of Life Questionnaire Followed by Paper-Based Questionnaire for the Non-Responders: Daily Practice in Patients with Prostate Cancer. Int Jnl Cancer Clin Res 2015, 2:2 ISSN: 2378-3419 DOI: 10.23937/2378-3419/2/2/1015
7. Basch E, Iasonos A, McDonough T, Barz A, Culkin A, Kris MG, Scher HI, Schrag D. Patient versus clinician symptom reporting using the National Cancer Institute Common Terminology Criteria for Adverse Events: results of a questionnaire-based study. Lancet Oncol. 2006 Nov;7(11):903-9. doi: 10.1016/S1470 2045(06)70910-X. PMID: 17081915.
8. Tillier CN, Boekhout AH, Veerman H, Wollersheim BM, Groen PAM, van der Poel HG, van de Poll-Franse LV. Patient-Reported Outcome Measures compared to Clinician Reported Outcomes regarding incontinence and erectile dysfunction in localized prostate carcinoma after Robot Assisted Radical Prostatectomy: impact on management. Accepted for publication (Urology Oncology: Seminars and Original Investigations) Augustus 2023
9. N. Grivas et al. Quantitative assessment of fascia preservation improves the prediction of membranous urethral length and inner levator distance on continence outcome after robot-assisted radical prostatectomy. Neurourology and Urodynamics. 2018;37:417–
425. DOI: 10.1002/nau.23318
10. Tillier CN, Vromans RD, Boekhout AH, Veerman H, Wollersheim BM, van Muilekom HAM, Boellaard TN, van Leeuwen PJ, van de Poll-Franse LV, van der Poel HG. Individual risk prediction of urinary incontinence after prostatectomy and impact on treatment choice in patients with localised prostate cancer. Neurourol Urodyn. 2021 Aug;40(6):1550-1558. doi: 10.1002/ nau.24703. Epub 2021 May 18. PMID: 34004044.
11. Williams, T.R., et al., Incidence and imaging appearance of urethrovesical anastomotic urinary leaks following da Vinci robotic prostatectomy. Abdom Imaging, 2008. 33(3): p. 367-70.
12. Tillier C, van Muilekom HAM, Bloos-van der Hulst J, Grivas N, van der Poel HG. Vesico-urethral anastomosis (VUA) evaluation of short- and long-term outcome after robot-assisted laparoscopic radical prostatectomy (RARP): selective cystogram to improve outcome. J Robot Surg. 2017 Dec;11(4):441-446. doi: 10.1007/s11701-017-0677-1. Epub 2017 Jan 12. PMID:28078524.
13. Vromans RD, Tillier CN, Pauws SC, van der Poel HG,van de Poll-Franse LV, Krahmer EJ. Communication, perception, and use of personalized side-effect risks in prostate cancer treatment-decision making: An observational and interview study. Patient EducCouns. 2022 Aug;105(8):2731-2739. doi: 10.1016/j.pec.2022.04.017. Epub 2022 May 4. PMID: 35534301.

