Assessing the needs of cancer survivors
Health services are continuously being put under pressure to deliver five-star service; with patient demand increasing and the lack of financial support and resources, this proves more and more difficult.
The only way to meet such demands is by radically changing how we currently practise, and revisit our patient treatment pathways to make them more efficient and effective for both patient and hospitals.
We know more people are surviving cancer because of early diagnosis and improved treatments. However, from patient satisfaction surveys and National Patient Reported Outcome Measures (PROMs) many cancer survivors are living with moderate to severe unmet needs (Macmillan, 2014). Marsh (2014), states “We have achieved most as surgeons when our patients recover completely and forget us completely.” The question we need to ask ourselves is this: If patients are experiencing unmet needs how can they move on with their lives and put their cancer care behind them?
The UK has implemented the ‘Recovery Package’ as a national recommendation from The National Cancer Survivorship Initiative (2007). The aim is to implement key interventions to identify the unmet needs of patients in specific tumour sites. By gaining this knowledge and understanding of patients’ concerns and problems, professionals can provide tailored support, education and intervention for their patients. If patients are physically and psychologically supported, educated and learn to cope and manage the after effects of their treatment and disease they will feel more empowered to self-manage and will want to live a more healthy and active life.
Recovery package
Three key areas of the recovery package we have focused on in our hospital are the following:
Holistic Needs Assessments
A Holistic Needs Assessment (HNA) is a questionnaire that is completed by patients affected with cancer, and identifies the patient’s physical, emotional, spiritual, practical and social needs and concerns. The aim is to address these unmet needs within an acceptable timeframe by sharing these unmet needs amongst the multidisciplinary team to improve patient’s management and care.
In the UK, HNAs are recommended to be completed at the following points of the patients pathway; start of treatment, during treatment, end of treatment, Health and Well-Being Events Health and well-being events are events aimed at supporting patients through their treatment by involving different members of the multidisciplinary team to actively provide education, support or signposting people to the appropriate resources or support services. The events are tailored to your patient’s cliental and tumour specific needs and concerns. Patients’ biggest concerns or unmet needs are identified from the HNA questionnaires, which devised the content of what should be included in the health and well-being events.
Treatment Summaries
A treatment summary is a letter sent to the commissione medica locale or primary care doctors. The aim is to provide information on what treatment the patient has had in hospital and to give instructions on any interventions, for example, on-going medication or clinical observations. The treatment summaries also help the patient to understand what to expect in the future including; late side-effects and possible treatment toxicities, future management plan and the contact details for health professional to answer any future concerns.
These key elements of the recovery package aim to support and encourage self management.
“The seminar sessions have also been more efficient and effective for the healthcare professionals. Conducting one to two-hour group sessions has reduced the waiting list in the outpatients clinic because the nurses can now see up to twentyfive patients at once.”
Survivorship pathway for prostate cancer patients
In a busy urology unit in the UK, in 2014/15 we treated 1,500 prostate cancer patients. The only way to deliver these three elements of the recovery package we needed to devise a new survivorship pathway for prostate cancer patients. We ran several focus groups; for patients, specific ethnic groups and health professionals to establish what patients wanted from us. Also establishing what was feasible from the multidisciplinary team regarding time and commitment as there is currently no extra finances or resources associated with the recovery package. The following pathway was blueprinted:
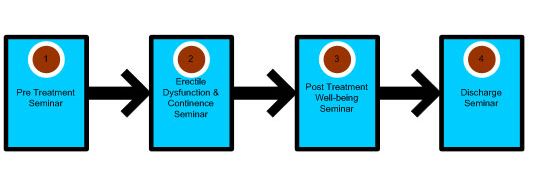
Four seminar sessions have been embedded in to the prostate cancer survivorship pathway.
Seminar 1 Pre Treatment Seminar
This seminar is compulsory for all patients that are going to have prostate cancer treatment at our hospital. The pre-treatment seminar session physically and psychologically prepares patients for their pending treatment and enhances self management, educating them on their disease, side effects or complications they may experience during or after their treatment. There is also a key focus on healthy eating and physical exercise to promote life style changes. Each seminar session is tailored to the different treatments.
Seminar 2 Post Treatment Erectile Dysfunction (ED) and Continence Seminar
The erectile dysfunction and continence seminar is compulsory for all patients who have had robotic surgery. They attend this seminar four weeks after their catheter is removed to be educated on pelvic floor exercises, ED and a demonstration for using the vacuum erection device (VED).
The HNAs highlighted that ED and continence were among the biggest concerns and unme diagnosis of recurrence and transition to palliative care. needs for our patients which is why this seminar was implemented.
Seminar 3 Post-Treatment Well-being Event
This is the only seminar we have not made compulsory based on the feedback from patients. Patients felt seminars 1 and 2 informed and taught them self management and coping techniques for their side effects and signposted them to other resources if they required any further interventions. However, we do still run a post-treatment wellbeing event for patients that have expressed any concerns that need more support physically or psychologically.
Seminar 4 Discharge Seminar
The discharge seminar is also compulsory for all patients that are being discharged back to their commissione medica locale or primary care doctors for follow-up. This seminar is aimed to encourage and empower patients to take back responsibility for their own health and future follow-up appointments. The seminar is designed to show patients what resources are in the community, help provide peer support and ensure they understand their future follow-up regime with their commissione medica locale or primary care doctors.
Evaluation
The new pathway has been successful not only for patients but also more cost efficient and effective for healthcare professionals. Delivering interactive group seminars has opened communication channels between patients, healthcare professionals and community services. All patients who have attended a seminar have completed a feedback questionnaire, and the majority of the patients found the seminar beneficial.
A total of 97% of patients who attended the seminars felt they benefited and gained more knowledge and coping strategies and 100% of patients were satisfied with the seminars. One of the biggest impacts to the group seminars was peer support; patients found it comfort in knowing other people were in the same situation and there were resources that could help them cope. The seminar sessions encouraged patients to ask questions about personal problems and also helped patients who were too embarrassed to ask personal questions as the group discussions were reported back as having a relaxed atmosphere and put people at ease. One patient said: “All the questions I wanted to ask but was too embarrassed to were either addressed by the nurses or another patient asked the question.”
The seminar sessions have also been more efficient and effective for the healthcare professionals. Conducting one to two-hour group sessions has reduced the waiting list in the outpatients clinic because the nurses can now see up to twenty-five patients at once. This new survivorship pathway has also reduced the number of outpatient’s appointments for patients, and has allowed healthcare professionals more time to provide efficient service to their patients.
By Paula Allchorne,, MBA, Dip, RGN (UK), Guy’s Hospital, Dept. of Urology, London (GB)
European Urology Today Vol. 28 No. 1 January/February 2016

