First ever urotherapeutic Guideline
Prostate carcinoma (PCa) accounts for 25.4% of all the types of cancer diagnosed in males in Germany. 60,000 males in their mid-60`s are diagnosed with PCa every year. The overall age is approximately 69 years. By 2050, the male population over the age of 60 is estimated to rise to approximately 28 million (37% of the total population), which is expected to result in the same proportion of increase of PCa patients.
This rise in PCa patients will have to be supported through diagnoses, therapy and post- treatment (Lorch, Alberts 2015). The choice of therapy for locally restricted and locally advanced prostate carcinoma is radical prostatectomy (Wirth, Fröhner 2014).
Although many experts consider this form of therapy to be the best, there are risks involved, which can lead to various post- operative restrictions. Despite being free of the tumour, post- operativequality of life (QoL) plays an important role in rating the therapy success. Changes often experienced by patients include bladder incontinence and erectile dysfunction, as well as general health problems such as fatigue and sleep disorders. They often notice an increase in emotional burdens before the therapy begins. It is important to discuss these problems early with the patients and to advise them of possible solutions. Adequate advice regarding fears and side effects of the therapy is the ground work for the full treatment concept (Holze et al. 2012). Urotherapists can contribute to a positive outcome with counselling, education and guidance during the pre-operative phase, as well as during the treatment process.
Urotherapeutic guidelines
It was our goal to develop the first guideline not only for the urotherapists involved in the therapy of locally situated PCa, but also for others involved in the therapy for patients and their carers or relatives.
In addition, the guidelines serve to make the work of the urotherapists transparent and reviewable within the multi-disciplinary team. For this reason not only urotherapists with nursing expertise but also physiotherapists, nursing scientists, urologists and patients have contributed valuable input to these guidelines.
Therapy and QoL
Regarding the post-operative limitations, despite the operating methods to reduce damage to nerves, urotherapeutic treatments become more meaningful for all those connected to the recovery process because of the increase in cases. With advice, education and training already in the pre-operative phase and during the whole period of the treatment, urotherapists can make an important contribution to the treatment process by fostering coping strategies and supporting affected males to improve QoL.
The guideline is based on the means of treatment and collaborates the results of medically indicated therapy carried out as well as questions on subjects such as food, skin care and assistance. The aim is that patients receive assistance in urotherapy in all phases of overcoming the illness.
Urotherapeutic education uses aspects of cognitive behaviour therapy and fundamentals in theoretics teaching in order to support people to adapting to their condition.
Various prostate centres in Germany offer urotherapeutic guidance to patients. The guideline offers assistance to the medical personnel involved, including urotherapists. Professionals’ pre-operative counselling and education are given to the patients before the pain from the operation causes limitations. This includes specific exercises in awareness of pelvic floor, perception and training contraction muscle control in order to actively help the recovery process.
Individual needs change the course of treatment “Specific situation/right time” is key for the treatment guideline (Wenneberg et al 2001; National Institute for Health and Care Excellence (Nice) 2021).
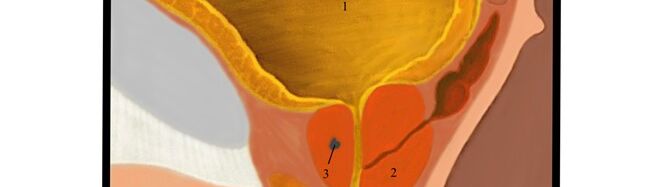
During the pre-operative phase, the cancer illness and unwanted side effects of the operation are foremost. Most often it is best that patients attend extended patient-education in a clinic for approximately two weeks before the operation for educational instruction. In this time, anatomy and psychology of the excretory and sexual organs, as well as pelvic floor, are discussed with patients.
Knowledge regarding the ability to regulate areas in the lower body or to rest are shared. The training should deal with pelvic floor activity such as retracting and relaxing, continence training, breathing exercises, post-operative instructions in standing, and lower leg exercises to prevent thrombosis risks.
This is the time to offer psychological guidance and sexual therapeutic advice. Post-operative information regarding suppression of excretory, as well as further examinations are required. Patients are dealing with a new life changing situation with the awareness of a new masculinity (Kong et al. 2017). In this post-operative time the individual needs of patients should be discussed, such as: current and future behaviour goals; and further advice and guidance in catheter care, skin care, and assistance. Advice on drinking, eating, toilet visits (including the positioning of the toilet), as well as pelvic floor/ micturition training, are also discussed. Relaxing methods and also sport activities are part of this individual advice.
Patients experience physical, sexual, and social changes, as a result of the operation and the cancer disease. This must be dealt with in the rehabilitation period. Information in follow-up treatment can be integrated according to the needs of the patient. During all patient contact the urotherapist has questions about the actual wellbeing. If necessary, contact with other members of the multi-disciplinary team can be arranged (e.g. urologist, physiotherapist, psychological oncologist, social worker).
Quality of life and patient education
Every patient has the right to comprehensive rehabilitation, and voluntary participation in urotherapeutic guidance is recommended for the wellbeing of a PCa patient. Urotherapeutic education is essential in order to enable patients to deal with daily side effects experienced with PCa. Additionally, addressing psychological and social challenges, as well as a successful return to work (Heuveling 2021), are essential components of the patient’s holistic care.
As a result of a cancer diagnosis and dealing with coping strategies some patients forget the information received during the initial treatment time. For this reason, now is the right time to repeat information and discuss individual problems within a multi-disciplinary team or to make appropriate support available to those affected.
Conclusion
The guideline is a unique treatment suggestion for all involved in the education for patients before and after a radical prostatectomy with non-invasive PCa. It describes the urotherapeutic options for patients, their carers and relatives in all phases of treatment with the assistance of a urotherapist, and a multi disciplinary team.
Here is the PDF of the full Urotherapeutic guideline.
—
Mrs. Barbara Schilcher, Urotherapist, Guideline coordinator, D-A-CH Association of Urotherapy e.V., Halle (DE)
Mrs. Doris Scholt, Nurse – Intensive care and anaesthesia specialist, D-A-CH Association of Urotherapy e.V. Halle (DE)

