Implementing patient-reported outcome measures (PROMs) in clinical practice
The Netherlands Cancer Institute (NKI) is a comprehensive cancer centre in Amsterdam. Patient-reported outcome measures (PROMs), or standardised questionnaires about health-related quality of life (HRQOL), were implemented in 2021 at the NKI for use in the outpatient clinics. We aim for healthcare providers (HCPs) to discuss patients’ completed PROMs with them during outpatient consultations to better align care and supportive care with patients’ needs.
We invite patients at set times before, during, and after treatment to complete PROMs. Patients areinvited by their HCP through the electronic health record (EHR); future questionnaires are triggered automatically after initial invitation. Patients complete PROMs through the EHR’s patient portal. Currently, cancer patients from 10 various types of cancer are invited to complete PROMs. About 70% of patients complete baseline PROMs, and 56-70% complete follow-up measurements.
Electronic health records
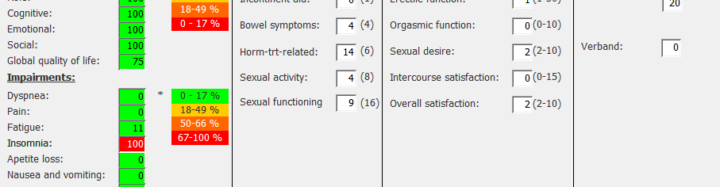
Patient’s PROMs are automatically saved in the EHR and the outcomes are presented on a dashboard. We can see the outcomes of several PROMs over time in a graph, enabling us to inspect trends in scores. We have applied thresholds of clinical importance [1] to facilitate interpretation of the scores: scores that are worse than the thresholds are reported in red, scores that are better are reported in green. This facilitates a quick overview of scores that require clinical attention.
Personalising care
Upon discussing PROMs, HCPs can refer patients to clinical and non-clinical supportive care services. However, if they are unsure which referral to make, they can ask for triage by a specialised supportive care nurse at the NKI ‘Centre for Quality of Life’ [2]. In one or several consultations, these nurses can unravel patients’ supportive care needs and propose fitting comprehensive care recommendations. We are currently also implementing self-support tools and recommendations in the PROMs dashboard, including patient information, self-help apps, eHealth tools, and decision-support tools that the patient can access upon discussing their PROMs with the HCP.
Experience from NKI
In the Urology Department, PROMs have played a fundamental role for 10 years already, particularly in the field of prostate cancer (PCa). PROMs are taken into account in shared decision making (SDM) and in routine clinical follow-up to monitor the side effects of treatments from a patient’s perspective. The PROMs patients complete questionnaires are validated: EORTC QLQ-C30, EORTC PR-25, IPSS, ICIQ-SF, and IIEF. PROMs are completed online. In case of non-response, a paper version is sent to patients. The response rate is high: 90% before any treatment, and 77%, 86% and 82% at 6, 12 and 24 months after prostatectomy, respectively. [3]
Shared decision-making
Several treatment options are available at the NKI for men diagnosed with primary localised PCa, including radical prostatectomy (RP), external beam radiotherapy, brachytherapy, and active surveillance. Many men with localised PCa are referred to our institute for treatment. PCa patients complete PROMs before their first consultation. Some patients have a preference for brachytherapy or for neurosafe prostatectomy. Following a patient’s PROMs, we can explain that brachytherapy is not an option due to lower urinary tract symptoms, as shown in the example above (IPSS of 20). The QLQ-C30 questionnaire also gives an indication of the patient’s physical and mental condition.
Of course, the final treatment decision is not based solely on the PROMs. Clinician reported outcomes (CROs) and patient preferences are also taken into account. In the example above, a patient may have an IIEF-EF score of 1/30, which does not necessarily mean that he has low erectile functioning. On further questioning the patient, it may be that the patient has not been sexually active in the last month, but has a normal erection. This patient could then opt for a neurosafe prostatectomy.
PROMs after RP
The most bothersome side effects of radical prostatectomy (RP) are urinary incontinence and erectile dysfunction. The NCI sends PROMs out at 6, 12, 24 and 36 months after RP. We recently demonstrated the impact of discrepancy between PROMs and CROs after RP. [4] Urinary incontinence was underreported by clinicians and the clinician over-reported the recovery of erectile function. Our study underlined the importance of discussing PROMs with patients during the follow-up consultation.
Practice experience
Ms. Tiller: “I have to admit that I use the PROMs during the follow-up after RP for more than 10 years. I have 10 minutes for each consultation and it does not take more time to address the PROMs in the conversation with patients. I always discuss the abnormal scores of the PROMs with patients; however, I also check whether the “good” scores match the patient’s physical and mental condition. From my experience, I have noticed that patients are satisfied that PROMs are discussed in the consulting room.”
—
Ms. Corinne Tillier, Nurse practitioner, PhD candidate, Netherlands Cancer Institute, Amsterdam
Ms. Kelly De Ligt, Post-doctoral researcher, PROMs implementation lead, Netherlands Cancer Institute, Amsterdam

