Improving follow-up care after nephrectomy

Similar to worldwide trends, renal cell carcinoma (RCC) in the Netherlands comprises 2% of all the malignancies1. The Netherlands Cancer Institute is a specialised institute where many cases of nephrectomies and partial nephrectomies are performed in localised and locally advanced RCC.
The follow-up after surgery was until 2014 done by the urologists only. There were no common guidelines for the follow-up. In 2014 we decided to develop a standardised follow-up after partial and total nephrectomy where the clinical nurse specialist could play an important role. The goal was to have a standardised follow-up and to decrease the consultations by urologists.
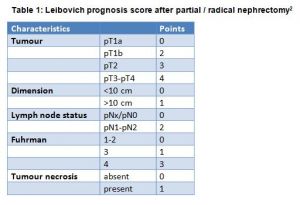
We evaluated that performing the follow-up alternating with urologist and a clinical nurse specialist could generate a decrease of the urologist’s consultations by about 58%. We decided to include the Leibovich prognosis score2 which is dependent of the risk of recurrence in order to perform an adapted/personalised follow-up after partial or radical nephrectomy. The score takes into account the pathological T stage, nodal status, tumour size, nuclear grade and histological tumour necrosis. The Leibovich prognosis score gives a score ranging from 0 to 11 and is categorised into three groups dependent of the risk of recurrence after surgery: low- (0–2), intermediate- (3–5) or high-risk (≥6) groups (Table 1).
We implemented a standardised follow-up according to the evidence based in August 2015. We divided the patients into three groups depending on the risk of recurrence after partial/radical nephrectomy (low, intermediate and high-risk groups). The follow-up is alternately done by the urologist and the clinical nurse specialist urology. The follow-up after partial nephrectomy and nephrectomy is, respectively, five and nine years. Four weeks after the surgery, the patient has a consultation with the urologist who explains the risk of recurrence and reviews with the patient the medical issues one month after surgery. The patient receives from the urologist an overview of the follow-up for the next years. A few days after the clinical nurse specialist calls the patient and asks if everything is clear. The nurse explains his/her role in the follow-up as the permanent contact person who is accessible for the patient when needed.
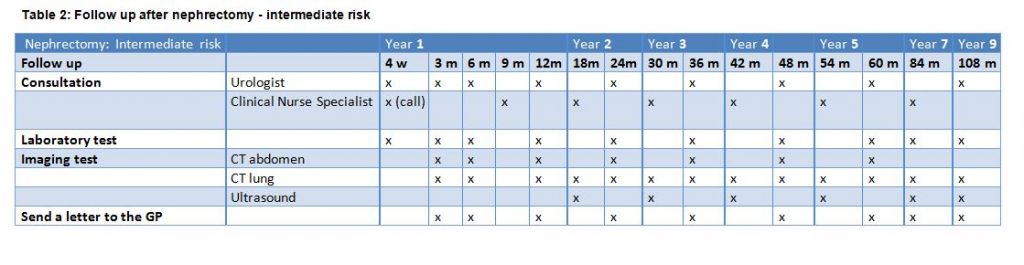
Table 2. Follow-up after nephrectomy – intermediate risk
A personalised follow-up depending on risk of recurrence is linked with the digital file of the patient (Table 2). This means that all the requests for CT scans, ultrasounds and blood tests are computerised. The urologist or the clinical nurse specialist has to fill at the time of the follow-up (for example month 42) and all the imaging tests and laboratory tests needed for the next consultation are automatically included and scheduled (Table 3). If the patient develops metastasis during the follow-up, we end the follow-up in the digital file and we refer the patient to the oncologist.
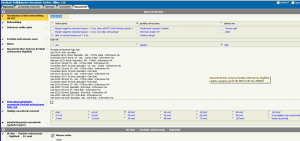
Table 3: Example of computerised orders
Preparing for the consultation (Self-Management)
During the follow-up, the patient has the opportunity to prepare the consultation with the urologist or clinical nurse specialist. The patient can log-in through his patient portal (www.mijnavl.nl) and can ask questions or report physical/mental complaints after surgery. When the urologist/nurse clinical specialist prepares the consultation (a few days before), the questions/complaints appear in the complaints are: Is my cancer hereditary? Is it normal that I am still very tired? Do I have to follow a special diet after phrectomy? Can I live with one kidney without health problems?
The patient is very satisfied to have the opportunity to prepare her/his consultation because in this way the patient will remember to ask a question to the urologist/clinical nurse specialist. We have to admit that we are also very satisfied since it makes the consultation easier. We can already prepare the answers to the questions/complaints. We have evaluated the follow-up after partial or radical nephrectomy (one year after implementation).
The patient expressed satisfaction on the following:
• The alternating consultation urologist/clinical nurse specialist. They do not mind who is giving the results of CT Scans/ultrasounds/ laboratory results;
• Receiving a schedule of the visits for the next five to nine years;
• Having the same urologist/clinical nurse specialist; and
• Having the opportunity to prepare the consultation.
The urologist has fewer consultations after partial/radical nephrectomy (for example 28% less consultations for low-risk after nephrectomy). We noticed that compared to the follow-up before the standardisation, we perform less CT scans. Moreover, the clinical nurse specialist appreciates providing counselling and support to the patients and is able to give the results of the CT scan or other exams.
Feasible scheme
The personalised follow-up after partial and radical nephrectomy based on the Leibovich prognosis score is feasible, efficient and can be alternatively done by the urologist and the clinical nurse specialist. It saves consultation time for the urologist and also reduces financial costs (less CT scans). The computerisation of the orders depending on the moment of the follow-up avoids unnecessary CT scans and allows a standardised follow-up.
References
1. Dutch Cancer Registration 2015: http://www.cijfersoverkanker.nl/selecties/Dataset_2/img578bcb8073d2d
2. Leibovich BC, Blute ML, Cheville JC et al. Prediction of progression after radical nephrectomy for patients with clear cell renal cell carcinoma: a stratification tool -for prospective clinical trials. Cancer 2003; 97: 1663–71.
Corinne Tillier, CNS, MANP, Clinical Nurse Specialist Urology, The Netherlands Cancer Institute, Amsterdam (NL), c.tillier@nki.nl

