Nurse-led flexible cystoscopies
As a nurse cystoscopist, some of the most vital aspects in care management of surveillance patients with non-muscle invasive bladder cancer (NMIBC) include continuity of care, timely follow-up, and having a specific point of contact. These allow patients to have trust and confidence in the management of their disease.
I carry out a weekly flexible cystoscopy list solely for NMIBC patients who require surveillance post treatment and have undergone transurethral resection of bladder tumour, intravesical Bacillus Calmette-Guérin (BCG), chemotherapy and radiotherapy follow-up. This group of bladder cancer patients requiring surveillance are unique; they adhere to strict follow-up guidelines and need regular surveillance flexible cystoscopies, which can lead to lifelong care.
Hospital attendances can involve the fear of the cancer recurring, anxiety and worry about pain. Having spoken to regular surveillance patients, I am aware that they find comfort in knowing they see the same person every time they go to the clinic for their flexible cystoscopy. The doctors’ posts continually change and their clinical demands are high. Having a nurse cystoscopist, whom the patients already know perform the “dreaded check cystoscopy”, can reduce their anxiety.
There are no studies specifically dedicated to determining patient anxieties regarding nurse-led flexible cystoscopy. Data from a personal cohort initially demonstrated that 97% of patients said that they were happy with a nurse specialist to perform the cystoscopy again in the future. The 97% became 100% as the patient who was unsure at first changed his mind, and confirmed that if the same nurse performed the procedure, he would be more than happy.
As a specialist bladder cancer nurse, I feel fortunate to meet the patients at the beginning of their bladder cancer journey – from initial diagnosis, administration of intravesical treatments, to surveillance flexible cystoscopy (if that is the follow-up route taken).
Questions have been raised about the costeffectiveness of nurse-led flexible cystoscopy. Historically, it has been documented that a nurse may not see as many patients as a doctor would, but this number will increase as the nurses gain more experience. It has also been recognised that nurses can be trained to carry out cystoscopy and identify abnormalities as accurately as urologists could. It could be argued that the nurse provides a more holistic approach by allowing more time for their consultation.
During my cystoscopy consultations, I always ensure that the patient understands the procedure and feels relaxed. When needed, I distract them by engaging in different topics of conversation unrelated to the procedure. I recommend to let patients watch a cystoscopy video and give them as much or as little information as they require, based on the assessment during the preliminary meeting. When patients have sufficient preparation, psychological care, continuity, and a point of contact, I am confident that nurse-led surveillance cystoscopies can significantly reduce their anxieties.
Certainly in the United Kingdom, only senior and experienced clinical nurse specialists should be selected for flexible cystoscopy training as specified in the British Association of Urological Surgeons (BAUS) and British Association of Urological Nurses (BAUN) guidelines. It is recommended that the nurse will have had two years’ experience in urology and have the support of a consultant urologist to undertake flexible cystoscopies. This is imperative for the training process to be successful.
During training, it is advised that a nurse completes a comprehensive in-house training programme led by a consultant urologist. Additionally, they should demonstrate their knowledge and competence by completing a training booklet and undergoing assessment, so both nurse and consultant urologist are satisfied that the nurse can work independently.
The Training Tool I used was adapted from the BAUN/BAUS guidelines and endorsed by the local trusts clinical governance team and the heads of nursing and urology department. The tool was divided into four sections. These were: Theoretical, Observational (minimum 10), Practical (minimum of 50 supervised as recommended by BAUN), and Consolidation of practical competence (30 unsupervised) with confirmation of the accuracy of findings overseen by the supervising urologist. These findings were retrospectively reviewed using video data to ensure consistency. A nurse cystoscopist report was devised for the nurses’ portfolio to keep a log and evidence of training using video cystoscopes.
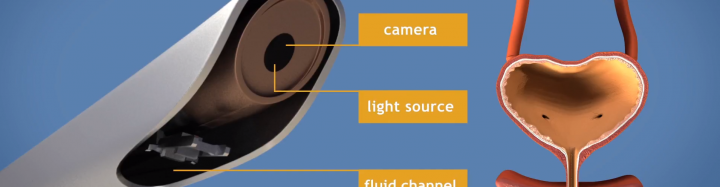
The theoretical component comprised of a Self-Directed Learning Package which includes the anatomy and the physiology of the bladder; investigations of haematuria; bladder cancer overview; principles and workings of a cystoscope; complications and antibiotic prophylaxis; follow-up protocol; and up-to-date literature for reference.
Are you interested in learning how to be a nurse flexible cystoscopist? Do you want to provide high quality service, and consistency for your patients? Or would you like to know how to hold a scope and learn the principles of cystoscopy? Come and join us at the flexible cystoscopy workshop at the 20th International Meeting of the European Association of Urology Nurses (EAUN19) in Barcelona. Grab the opportunity to learn the basics and apply your new skills in your local hospitals.
Chatterton Kathryn, BSc (Hons), Bladder Cancer Clinical Nurse Specialist, Guy’s and St Thomas’, NHS Foundation Trust, London (UK), kathryn.chatterton@gstt.nhs.uk

