Thought-provoking session about post-RALP rehabilitation
Amsterdam 2022 was my first experience of attending the EAUN congress. I feel honoured that the EAUN selected me for a travel grant of €500. This enabled me to take part in this wonderful event. The programme was varied, providing stimulating, thought provoking and inspirational presentations. The opportunity to network and collaborate with other professionals from Europe and beyond provided insight into the world of urological nursing. This led to interesting comparisons of nursing roles and scopes of practice.
Topics that are overlooked
‘Treatment of Prostate Cancer’ was a topic that related most to my current role as uro-oncology nurse specialist. The presentation addressed topics that are often overlooked and focussed on the longer term potential side effects of individual treatments. In particular, the focus on erectile dysfunction following robot-assisted laparoscopic radical prostatectomy (RALP) was extremely interesting and relevant to my practice. My ‘penile rehabilitation’ clinic allows for men post-RALP to partake in a programme aimed at addressing any loss of sexual function following surgery. The presentation stressed the importance of penile rehabilitation, an aspect of after–care that was often ignored. Although I agree wholeheartedly with the importance of rehabilitation, I feel that surgeons are very good at asking about sexual function at post-operative reviews and then refer patients to the clinic.
Factors such as ‘time’ and ‘effort’ were addressed during the presentation. This is something that I discuss from the outset, allowing for the management of patient expectations and commitment, always reinforcing that there is no ‘immediate solution’.
Pelvic floor management for erectile dysfunction
Pre-operative counselling, which is also part of my role, allows for the opportunity to discuss post-RALP side effects, such as urinary incontinence and erectile dysfunction. Interestingly, the importance of pelvic floor management and its relevance to sexual function were also addressed during the presentation. In my practice, when patients are listed for RALP surgery they are automatically referred to the physiotherapist who specialises in pelvic floor dysfunction.
Timing of rehabilitation was also discussed. It was deemed that the use of a vacuum erection device (VED) should ideally be initiated 6 weeks post- surgery, once the catheter has been removed. Although a brief mention of the option to pursue rehabilitation occurs during pre-operative counselling, the reality is that patients often cannot be seen in clinic for weeks, even months postsurgery. For a small minority of patients, rehabilitation may not be initiated for several months due to factors such as urinary incontinence, missed opportunity/referral or for a variety of personal reasons. The presenter reinforced that erectile dysfunction was equally as important an issue as urinary incontinence.
Not that important?
The idea is that patients are often focussed on their surgery and cure preoperatively and often see erectile dysfunction as something of secondary significance. I agree with this statement to some extent, as often the patients who delay the initiation of rehabilitation are the ones who do not put as much value on their quality of life post-operatively and who focus much more on ‘being cured’.
Our department decided to initiate discussion of the rehabilitation programme during pre-operative counselling, in order to allow the opportunity for all RALP patients to initiate penile rehabilitation (avoiding the potential of delayed referral). That ay, the patient receives treatment along with clear, concise instructions and guidance from the outset. We feel that this gives patients the opportunity to commence the programme confidently and immediately after their catheter is removed. By early initiation of the rehabilitation programme, an element of hope may be provided as well as an improvement in quality of life, psychological benefits and better outcomes overall. It also allows for patient choice and equality. If patients decide not to pursue the programme, then at least they have been given the opportunity to discuss the important aspect of erectile dysfunction. Thus, our team ensures that this is not overlooked.
Combination approach
A variety of methods to treat erectile dysfunction were discussed. Although there appeared to be no set criteria, a combination approach was more favourable for a better and earlier recovery. This reflects the practice in my clinic where currently patients use a combination of VED and phosphodiesterase type 5 (PDE-5) inhibitors (if no contraindication is identified).
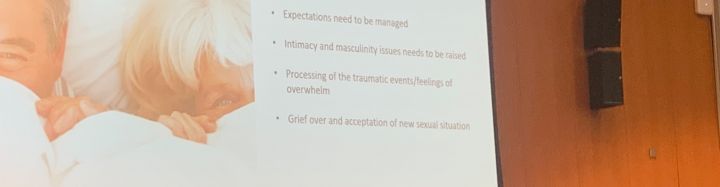
Interestingly, ‘talking’ was listed as a treatment approach. I agree that communication is crucial to every aspect of nursing care, in particular when discussing personal and often sensitive issues such as sexual function. Discussion with and education of the patient, ideally in conjunction with their partner, allows for improved commitment to the programme, acceptance of the new situation and better relationship dynamics. This undoubtedly avoids emotional distress, a sense of loss of masculinity/failure and thus allows intimacy to remain an important aspect of the patient’s life post-RALP, improving overall quality of life for some patients.
Overall, I found the presentation to be thoughtprovoking. It showed similarities with what I deliver in practice. It reinforced the need for communication and realistic expectations from the outset. Age, good pre-operative potency and nerve-sparing surgery were highlighted as being strong prognostic factors for the recovery of sexual function post-RALP. We do need to place emphasis on the statement that sexual function is an equally important issue as urinary incontinence post-RALP and should never be overlooked.
Ms. Danielle McManus, CNS Uro-Oncology, Knottingley (GB), danielle.mcmanus@nhs.net

