Using cannabis in prostate cancer patients
In our hospital’s daily practice we notice the popular use of cannabis oil in prostate cancer (PCa) patients. As a nursing specialist for urology, I have even met patients who are so convinced of the curative benefits of cannabis oil in treating prostate cancer that they replace standard treatment with the use of cannabis oil.
These patients include those who have localised prostate cancer where active surveillance is followed, those with biochemical recurrence after treatment, and patients with metastatic PCa. I have always wondered whether cannabis oil could indeed be a cure for prostate cancer. Unfortunately, I do not see in practice the desired beneficial effect and the PSA values continue to rise. To find some answers, I did a search in scientific literature.
 Cannabis, a very easy plant to grow, has been used for centuries for its medicinal properties. The oldest known document about cannabis use originates from the Chinese emperor Shen Nung in 2727 B.C. It suggested that cannabis has a neuron-protective effect. The Egyptians used cannabis to treat glaucoma and as an anti-inflammatory agent (inflammation of the eyes, fever). Cannabis was even used in obstetrics (mixed with honey) and the mixture was applied in the vagina to “cool” the uterus. In the Old Testament, there is also an account of God instructing Moses to make a holy anointing olive oil-based “Kaneh Bosm.”
Cannabis, a very easy plant to grow, has been used for centuries for its medicinal properties. The oldest known document about cannabis use originates from the Chinese emperor Shen Nung in 2727 B.C. It suggested that cannabis has a neuron-protective effect. The Egyptians used cannabis to treat glaucoma and as an anti-inflammatory agent (inflammation of the eyes, fever). Cannabis was even used in obstetrics (mixed with honey) and the mixture was applied in the vagina to “cool” the uterus. In the Old Testament, there is also an account of God instructing Moses to make a holy anointing olive oil-based “Kaneh Bosm.”
Cannabis contains more than 400 chemical components 80 of which contain cannabinoid components and 200 non-cannabinoids components. For medical purposes, cannabinoid substances such as THC (Delta-9-tertrahydrocannabinol), CBD (cannabidiol) and non-cannabinoid substances such as terpenoids and flavonoids are relevant.
Medicinal cannabis must be distinguished from recreational cannabis which is used to achieve a psychotomimetic state of ‘high’. Cannabis strains used for recreational purposes contain a higher THC and lower CBD ratio than cannabis for medicinal use. Usually two cannabis plants are used: cannabis sativa which has a higher THC concentration and cannabis indica which has a higher CBD concentrate. The flavonoids are known for their antioxidant and anti-inflammatory effects. The terpenoids are resins (oil) with a strong odour.
In the 1990s, the endocannabinoid system (ESC) of the body was discovered by Raphael Mechoulam, an Israeli professor of medical chemistry. The endocannabinoid system, a central regulatory system, is the body’s largest receptor system and is important to maintain the homeostasis of the body.
 Human beings produce their own cannabinoids (endocannabinoids) according to need and are not stored in the body. Like endorphins, the human body produces endocannabinoids in response to activities such as physical exercise (the high of runners might be due to endocannabinoids, not endorphins!).
Human beings produce their own cannabinoids (endocannabinoids) according to need and are not stored in the body. Like endorphins, the human body produces endocannabinoids in response to activities such as physical exercise (the high of runners might be due to endocannabinoids, not endorphins!).
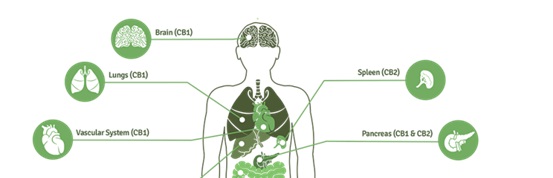
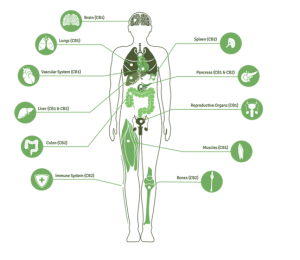
Cannabinoid receptor type 1 (CB1) is mainly found in the brain, and also in the lungs, the reproductive organs, etc. Cannabinoid receptor type 2 (CB2) is usually located in the immune system and in the bones. THC mainly works on CB1 receptors, CBD on CB2 receptors.
In vitro studies with THC have shown that cannabinoids affect migration, angiogenesis and apoptosis (programmed cell death) of cancer cells, but each type of cancer appears to respond differently to the effect of exogenous cannabinoids. Many types of cancer cells have a higher concentration of CB1 and CB2 receptors.
Use of cannabis in cancer
– Pain: Cannabinoids have been used for centuries to lessen pain. Historical texts and old pharmacopoeia noted the use of cannabis for menstrual cramps, pain during childbirth, and headaches. Studies have shown that the cannabinoids have no effect on acute pain and post- operative pain. Two placebo-controlled studies with a cannabis extract showed modest benefits when using cannabinoids in addition to opioids and other adjuvant pain-killers in cancer patients with chronic pain. However, the effect of cannabinoids in chronic neuropathic pain was clearly demonstrated in 29 randomized studies.
– Nausea and vomiting: An initial study in 1975 showed a beneficial effect of THC on nausea induced by chemotherapy. Subsequently, two systematic reviews showed benefits of cannabinoids in nausea and vomiting due to chemotherapy, but most studies were observational or uncontrolled.
– Stimulation of appetite: Cannabinoids seem to have only a modest effect in cancer patients with cachexia. More promising results were seen in studies in the population without cancer.
– Pre-clinical studies (in vitro = cells in laboratory and in vivo = in mouse model) have shown the antiproliferative, anti-metastatic, anti-angiogenic and pro-apoptotic effects of cannabinoids in various malignancies (lung, glioma, thyroid, lymphoma, skin, pancreas, endometrium, breast and prostate). Even if an identified substance in vitro / in vivo appears to have a beneficial effect on a disease, it is important to realise that only one in 5,000-500,000 substances obtain a registration and becomes available to the patient (after 10-16 years of different study phases). Cannabis has never been clinically studied as a treatment for malignancy.
 On the Internet, patients can get a lot of information about the curative effect of cannabis oil on prostate cancer but this information extrapolate the results of pre-clinical work to possible effects in people without any factual evidence. I often see patients in the doctor’s office showing me a website where it has been proven that cannabis oil can cure prostate cancer, which is obviously their own interpretation. In my view this can be a misleading message even though the website does not explicitly provide false information. The website [See figure below] shows information which is based on a study published in the British Journal of Cancer. This is correct, but the website “neglects” to mention that this is a publication of an in vitro study. The patient might not even know what an in vitro study is and is not aware that there are no studies on humans yet to prove this.
On the Internet, patients can get a lot of information about the curative effect of cannabis oil on prostate cancer but this information extrapolate the results of pre-clinical work to possible effects in people without any factual evidence. I often see patients in the doctor’s office showing me a website where it has been proven that cannabis oil can cure prostate cancer, which is obviously their own interpretation. In my view this can be a misleading message even though the website does not explicitly provide false information. The website [See figure below] shows information which is based on a study published in the British Journal of Cancer. This is correct, but the website “neglects” to mention that this is a publication of an in vitro study. The patient might not even know what an in vitro study is and is not aware that there are no studies on humans yet to prove this.
A challenge for the caregiver can be that the patient is convinced that we as healthcare practitioners work together with the pharmacists, and that we do not wish to carry out clinical trials (unfortunately, I hear that very often). We can hardly persuade patients that this is not true.
It is also important that we inform the patient about the possible interactions of cannabis oil with certain regular medications such as Coumarin (this blood thinner interacts with cannabis oil, leading to an increase of the INR and a greater risk of bleeding!). There are different types of cannabis oil available, such as CBD and THC oils with different concentrations which makes it difficult for patients to make a choice.
Conclusions:
• There is no proof of cannabis oil as cure for prostate cancer;
• It is important not to be prejudiced or judgmental against patients who use cannabis oil;
• Listening to the patient’s view can be helpful since the patient often confides to the nurse rather than to their physicians;
• Avoid persuading patients not to use cannabis oil, but try to convince them of the need to follow a regular treatment combined with cannabis oil;
and
• Consider adverse interactions between cannabis oil and certain medications and inform your patient about these.
References
- Abrams, D.I. Integrating cannabis into clinical cancer care. Current Oncology, 23, S8-S14 (2016).
- Benzi Kluger, Piera Triolo, Wallace Jones, Joseph Jankovic. The Therapeutic Potential of Cannabinoids for Movement Disorders. Mov Disord. 2015 Mar; 30(3):313–327.
- Bowles, D.W, O’Brien, C.L, Camidge D.R, Jimeno A. The intersection between cannabis and cancer in the U.S. Critical Reviews in Oncology/Hematology, 83, 1-10 (2012).
- Bridgeman M.B and Abazia D. T. Medicinal Cannabis: History, Pharmacology, And Implications for the Acute Care Setting. P T. 2017 Mar; 42(3): 180–188.
- De Petrocellis L. et al. Non-THC cannabinoids inhibit prostate carcinoma growth in vitro and in vivo:pro-apoptotic effects and underlying mechanisms. Br J Pharmacol. 2013 Jan; 168(1): 79–102.
- Guindon, J. Hohmann, A.J. The Endocannabinoid System and Cancer.: Therapeutic Implication. British Journal of Pharmacology. 163, 14447-1463 (2011) – Johnson J.R et al. Multicenter, dubbel blind, randomized, placebo-controlled, parallel-group study of the efficacy, safety and tolerability of THC: CBD extract and THC extract in patients with intractable cancerrelated pain. J.Pain Symptom Manage 2010;39:167-79.
- Machado Rocha F.C. et al. Therapeutic use of Cannabis Sativa on chemotherapy-induced nausea and vomiting among cancer patients: systematic review and meta-analysis. Eur. J. Cancer Care 2008;17:431-43.
- Olea-Herrero N. et al. Inhibition of human tumour prostate PC-3 cell growth by cannabinoids R(+)-Methanandamide and JWH-015: Involvement of CB2. British Journal of Cancer volume 101, pages 940–950 (15 September 2009).
- Portenoy R.K et al. Nabiximols for opioid-treated cancer patients with poorly-controlled chronic pain: a randomized, placebo-controlled, graded dose trial. J. Pain 2012;13:438-49.
- Ramos J.A. et al. The role of cannabinoids in prostate cancer: Basic science perspective and potential clinical applications. Indian J Urol. 2012 Jan-Mar; 28(1): 9–14.
- Tramer M.R. et al. Cannabinoids for control of chemotherapy induced nausea and vomiting: quantitative systematic review. BMJ 2001;323:16-21.
Corinne Tillier, Nurse Practitioner Urology, Antoni van Leeuwenhoek Hospital, Amsterdam (NL), c.tillier@eaun.org

