4. INDICATIONS, CONTRAINDICATIONS AND ALTERNATIVES TO MEC
MECs may be used as a relatively non-invasive means of male urinary incontinence containment. MEC are designed not to treat UI, but rather to contain the symptom of urinary leakage regardless of the underlying aetiology and as such constitute an important tool in the armamentarium for UI management.
Whilst not truly invasive in the strictest sense of the terminology, MEC are not without their complications, both common and infrequent and as such should be considered on a practical level to be minimally or relatively non-invasive.
MECs are designed to function as an external urinary conduit facilitating the capture, containment and external drainage of urine from the external urethral meatus, via standard drainage tubing into an external catheter bag which may be either strapped to the thigh or lower leg whilst ambulant or attached to a free standing device employed most commonly overnight or if significantly immobile or bed bound.
Adequate function of a MEC relies on several interval factors, the most crucial being adherence of the device to the penile shaft skin. Without effective circumferential water tight adherence, urine will leak through the imperfect seal at points of weakness or loss of adherance may occur and the patient’s symptom of UI will remain. It is vital, therefore to ensure that the MEC device is both sized and fitted properly to facilitate a good 360° seal.
This seal must not only be water tight but needs to be secure for an acceptable period of time for each individual patient. Some patients require containment with a MEC overnight whilst others may require a more sustained level of control and the MEC needs to be capable of remaining with excellent adherence for as long as required without losing strength.
Given the length of time a MEC remains in situ, both for each individual MEC and, as an often long term containment strategy, the device needs to afford an element of comfort for the wearer in order to facilitate compliance and longevity of function. Uncomfortable devices often lead patients to manipulate and handle the MEC in an attempt to improve wearer acceptability with the resultant effect of reducing adherence, urine leakage and device malfunction.
Skin integrity may become compromised by a combination of excessive or uneven adherence, frequent device change, lack of comfort and difficulty with applying or removing the MEC and patients and careers alike should be counselled and warned to keep a watchful look out for loss of integrity which usually requires the temporary abandonment of MEC use to facilitate healing.
Ease of application and removal are thus essential to the long term acceptability of MEC, and may also influence the decision regarding the onset of utilisation for those patients with reduced dexterity.
In summary, an effective MEC is one that stays securely in place for an acceptable period of time, is leak-free, comfortable to wear, easy to apply and remove, avoids skin damage, and channels the urine effectively into a drainage bag. [10]
Specific patient groups
Several distinct patient cohorts are worthy of special mention with respect to MEC usage on account of their often unique collection of pre-existing influential issues.
Older people with UI form, perhaps, the largest specific cohort requiring special consideration for several reasons. Changes with natural ageing mean that all types of UI become more common with increasing age and this is commonly associated with a combination of reduced mobility, limited dexterity, social isolation and impaired cognition. Specific interventions, such as assisted toileting may be required to successfully institute MEC containment is this group. [3]
Younger patients may also struggle with MEC usage, often for different reasons relating to body image or perhaps changing body habitus in those patients still physically maturing and this group requires specialised and empathic MDT management often involving psychological support.
Patients with restricted or impaired dexterity will require greater input to enable independent MEC use and to prevent inherent complications from inadequately applied devices and this group in common with the very young may require more intensive training and support than others to successfully manage their MEC.
Combining various kinds of continence management
For some men isolated containment with MEC may not be either the best or indeed the most personally acceptable option for all daily life situations and different but complimentary methods may be employed. For example, intermittent catheterisation may be necessary if the patient cannot empty his bladder voluntarily, or a MEC may be used during the day or during certain circumstances or activities whilst absorbents may be preferred overnight, particularly for those patients who are restless and may inadvertently avulse the device leading to skin and penile trauma.
4.1 Indications
The mainstay indication for containment with MEC devices is UI and as a containment product MEC devices should be considered only if other curative treatment options have either failed or are deemed unsuitable, perhaps on account of a patient being unfit for any other intervention or are requested by the patient.
The usual scenarios are
- Overactive bladder with urge urinary incontinence without a significant post void residual (PVR) urine in men.
- Men with UI and a significant post void residual urine who are incapable or unwilling to undergo any other treatment or intermittently catheterise, and in whom there are no other complications of chronic urinary retention.
Stress urinary continence as a consequence of external sphincter damage from prostatic surgery, (TURP, RRP) when further intervention e.g.: male sling or artificial urethral sphincter is either unsuitable of unacceptable to the patient. [11] - During periods of intense observation requiring strict fluid balance and an accurate knowledge of urine output when catheterisation is either unsuitable or impractical e.g.: extensive urethral stricture disease.
- UI in men with neurological disorders and neuromuscular syndromes.[12]
- UI in men with poor mobility, dementia, impaired cognition or impaired vision, or for whom accessing a toilet poses a safety issue.
For these latter indications, a social support or family network should be available to ensure that the MEC is used both appropriately and effectively with regular review to ensure its continued use is in the patient’s best interests. [13]
MECs may also be used for diagnostic purposes. [14] This falls outside the scope of these guidelines.
4.2 Contraindications
Contraindications to MEC are few and can be divided into absolute and relative.
Absolute contraindications
The only absolute contraindication to the use of MEC devices is the known presence of high pressure chronic retention which may be the underlying causative pathology of UI. Whilst the use of MEC devices in such a scenario may contain the symptom of UI, it will not influence the high intravesical pressure and resultant impact on renal function and as such a more invasive definitive therapy should be employed. [15,16]
The use of conventional cystometry will delineate the intravesical pressure but simple renal tract ultrasound scan will demonstrate the hall mark feature of bilateral hydroureteronephrosis even before a decline in renal function is manifest.
Relative contraindications
Relative contraindications are more reflective of the fact that most clinical scenarios are better managed with alternative means e.g. low pressure chronic retention or bladder atonia are better managed with either long term catheterisation or intermittent catheterisation but if these are unsuitable or if the patient insists, the use MEC devices are viable since the intravesical pressure is low and thus the upper renal tract is safe. With MEC devices however, the bladder, in these circumstances will fail to drain and increase the risk of UTI, stones etc., thus whilst possible, this containment method is far from ideal.
Other limiting and relative contraindications for the use of MEC include dermatological issues such as excoriated penile skin, psoriasis and localised allergy to materials used as well as cognitive impairment, as such patient, may traumatically avulse the MEC resulting in loss of skin integrity. [10]
Body habitus may form a relative contraindications for some patients as a consequence of a physical inability to apply the device or perhaps visualise the penis thus hindering adequate application. In general patients with a high BMI are at greater risk of this as a combined consequence of blocked vision due to abdominal girth and a prominent supra public fat pad causing loss of visible and accessible penile length upon which to place the MEC.
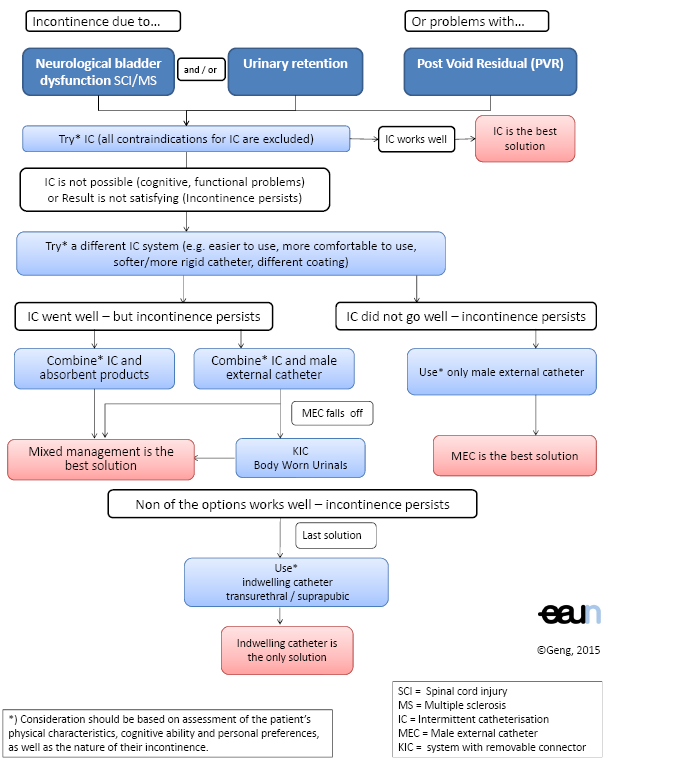
Flowchart 2. Management of incontinence with PVR - decision tree
4.3 Alternatives to MEC
Alternatives to MEC vary and largely depend upon the underlying cause of the UI necessitating the use of MEC devices. Patients suffering from overactive bladder should be offered the full range of therapeutic options available including lifestyle modification, pharmacotherapy and surgery if fit whilst those for whom prostate enlargement and bladder outflow obstruction is a causative factor bladder outflow surgery should be considered and offered.
Alternatives aimed at resolving or containing the actual symptom of UI include the following:
- Intermittent catheterisation
For intermittent catheterisation, a catheter is passed into the bladder via the urethra, urine is drained, and the catheter removed. This procedure may be utilised with variable frequency in patients who fail to empty their bladders completely. In certain circumstances some men suffer UI only at high bladder volumes and but are unable to void naturally, under such circumstances, timely intermittent catheterisation may lead to resolution of UI. [11,17]
- Absorbent products/pads
Absorbent containment products may be single use disposable or reusable washable products. They differ in size, width, shape and design as well as the volume of urine that can be contained without pad leakage. The material and additional aspects such as super-absorber components also help to reduce leakage as well as improve patient acceptability. Skin irritation akin to adult nappy rash (ammoniacal dermatitis), leakage and odour are problems associated with all absorbent products. In many health care systems such containment products carry a huge financial burden for the patient who may either be expected to purchase their own pads or may only be offered the poorer quality pads free of charge.
- Clamp/penile compression device
Clamps have been available for several decades but there are no published studies that have evaluated their safety, comfort or effectiveness. Clamps are an effective option, but for short periods only, and provided cognitive ability, manual dexterity and bladder and genital sensation enable safe use. [18] The complications of penile clamps include oedema, urethral or penile erosion, urethral stricture disease and ischaemia, and their use must therefore be approached with great caution. [19] The penile clamp is absolutely contraindicated in case of detrusor overactivity or low bladder compliance because of the risk of developing high intravesical pressure, and in the presence of significant urinary reflux. [12]
- Male sling
The male sling provides a suitable alternative to MEC for the treatment of stress UI, usually secondary to prostatic surgery e.g.: TURP, RRP and is indicated in this group for the treatment of mild to moderate UI. Patients who are deemed fit enough should consider this in preference to MEC. Complications include urinary retention, infection and device erosion.
- Artificial urethral sphincter (AUS)
In common with the male sling, the artificial urinary sphincter is an excellent alternative to the use of MEC devices in medically fit patients suffering from stress UI. The AUS is suitable for moderate to severe incontinence and has excellent reported efficacy, durability and patient satisfaction. Complications include infection, erosion and mechanical failure.
- Indwelling catheter
Indwelling catheters made of latex or silicone material are placed in the bladder, via the urethral or suprapubic route and are held in place with an intravesical balloon. An indwelling catheter is an invasive device and is associated with significant complications such as UTIs and encrustation of the catheter. [19] The indwelling catheter may improve quality of life because it frees patients from toileting and wet containment products. Indwelling transurethral catheterisation and, to a lesser extent, suprapubic cystostomy are associated with a range of complications producing considerable health problems such as an enhanced risk for UTI. Therefore their use should be restricted. [12,19] For further information, please refer to the EAUN guidelines “Catheterisation - Indwelling catheters in adults. [20]
